Worldcoronaviras has impacted different regions of the world differently. Low-income countries with weak healthcare systems have struggled to contain the spread of the virus.
COVID-19
Worldcoronaviras is an interactive data tool that allows users to track COVID-19 cases and deaths around the world. Country profiles are updated daily and show how the number of confirmed cases is changing. The charts also display how many new deaths have been reported and whether the death rate is rising or falling.
Global pandemics are always a serious threat to health. Viruses are known to spread rapidly and often have the ability to cause significant damage to organs, including the respiratory and vascular systems. Vaccinations and other prevention measures are crucial in reducing the number of cases and deaths.
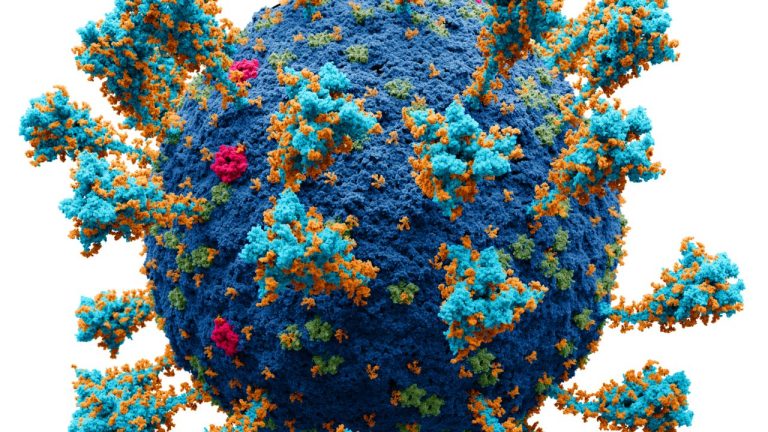
The WHO identifies coronaviruses as pathogens by their viral S1 subunit (S1 protein) that contains a receptor-binding domain (RBD). RBDs recognize the angiotensin-converting enzyme 2 (ACE2) receptor and are important for enabling a viral entry into a host cell. This receptor is found in a variety of animals, including human, pig, ferret, rhesus monkey, cat, pangolin, and rabbit11,43.
SARS-CoV-2 and other coronaviruses use different ACE2 receptors, which means that some of them are less efficient in activating this receptor than others. This can lead to differences in the way that SARS-CoV-2 is transmitted and how it affects people.
SARS-CoV-2 is a novel coronavirus that was first detected in China in 2003. It has been linked to the outbreaks of SARS and MERS and is the most recent member of a family of viruses with similar pathogenesis and host range. It is closely related to the bat SARS-related coronavirus RaTG13. This family of viruses is a major concern for public health in the Region and the World because it has the potential to cause severe disease, including pneumonia.
SARS
SARS is a disease caused by coronaviruses that spread easily among people, especially those who live or work closely together. It can cause severe breathing problems, often leading to respiratory failure and death in some cases.
Infection with SARS typically begins within a few days of exposure to the virus. It’s most likely transmitted through droplets that are released when a person coughs or sneezes. It also may be spread through contaminated objects, such as doorknobs and elevator buttons.
Most studies have found that SARS can be transmitted through close contact, including family members or health care workers. It can also be transmitted from infected to uninfected people through the air when someone who is infected coughs or sneezes.
The high transmissibility of SARS is probably a result of the unique virological features of the virus. It is highly transmissible during the asymptomatic phase or after illness onset, but less transmissible in patients who are already sick.
In a meta-analysis of observational studies, proximity to people who were infected with SARS-CoV or Middle East respiratory syndrome coronavirus (MERS-CoV) was associated with a lower risk of infection, particularly for people who lived close to infected individuals [262,292-294]. A distance of six feet or more was also associated with a reduced transmission rate, although this distance did not have the same effect on the asymptomatic transmission rate.
Despite these limitations, the risk of SARS can be minimized by avoiding situations where someone who is infected might be able to pass the virus. This can be done by staying away from places where people who are infected might congregate, such as schools and malls.
The virus is relatively stable on aerosols, but it can quickly inactivate when a person brushes against a surface that has been contaminated with the virus. It can also be inactivated by sunlight, which is why many countries have banned the use of airplanes for long periods of time after SARS has been reported.
MERS
MERS, also referred to as Middle East respiratory syndrome coronavirus or novel coronavirus (nCoV), is a virus that is part of a large family of viruses that can cause many different illnesses in humans. It is known to have a strong impact on respiratory health and can lead to severe symptoms such as pneumonia, breathing failure, kidney damage, high fevers, and death.
The virus is related to a group of coronaviruses called the betacoronaviruses. MERS-CoV belongs to the lineage C of this genus and has been identified in several species of bats in Europe, Africa, and China [3].
Dromedary camels are an intermediate host for MERS-CoV, and the virus appears to be transmitted from these animals to humans via contact with their saliva or mucus. Most cases have been reported in countries in the Middle East, including Saudi Arabia, United Arab Emirates, Qatar, Oman, and Jordan.
However, MERS-CoV has been detected in Europe and other regions with travel connections to the Middle East. In these locations, the virus has been transmitted from infected patients to others through direct contact with infected camels or in healthcare facilities.
Symptoms of MERS-CoV are flu-like and typically develop from 2 to 14 days after infection. People who have symptoms or have traveled to areas in the Middle East should see their doctor right away. They will get a chest X-ray, blood tests and kidney function tests.
Antiviral treatment isn’t available for MERS, but it can be helpful to help ease the symptoms and prevent further illness. It may also reduce the risk of complications such as pneumonia or kidney damage. It can be especially important for people with a more severe case of MERS-CoV who have rapid breathing, low oxygen levels in the blood and high fevers.
Hendra
Hendra is a bat-borne virus that can cause severe illness and even death in both horses and humans. It is also known to affect pet dogs, though the incidence of human infections is relatively rare.
The infection spreads via direct contact with respiratory emissions, like spit or blood drops, from a contaminated person and through contact with surfaces that are tainted with the virus. It can also be transmitted by a pregnant woman or her child during pregnancy or labor.
Vaccination is the only effective way to prevent this disease. It can protect horses and people from the risk of contracting this disease, although it is very important to remember that it does not necessarily prevent all cases of Hendra.
In Australia, the majority of people who get a case of Hendra virus from their horse are veterinarians and their staff. These people are in very close contact with the horse and they account for all but two of the confirmed human cases.
There have been many reports of vets leaving their profession, and some have stopped treating horses altogether because of the risk of contracting Hendra virus from their work. It is also a serious problem for owners who do not have their horses vaccinated and are therefore exposed to the disease when they come to the vets.
This is a very difficult situation for all parties involved. It’s especially hard for vets who are relying on their income from their work to survive. The costs of dealing with this disease are enormous. They include the cost of treating sick and ill horses, the cost of veterinary and public health services that have to deal with a large number of sick and injured animals, and the cost of transporting these animals from one place to another.
Rous Sarcoma
Rous Sarcoma, or RSV, is a type of human cancer caused by a virus. It is one of the first cancer viruses to be discovered, and it changed the way we think about cancer treatment.
While we have known for a century that some viruses can cause tumors in animals, we had no idea how they could do so in humans. Then, in 1911, Peyton Rous, a pathologist at the Rockefeller Institute in New York City, found a lump in a chicken that was growing into a sarcoma, and he began to wonder about the reason why this was happening.
In the course of his research, Rous uncovered some surprising discoveries about how this particular virus infects the body. He found that the virus binds to the cell nucleus and causes it to start copying its DNA, creating new cells in the process.
This process is referred to as reverse transcription. It is an exception to the central dogma of genetic theory, which states that information encoded in genes is always copied into a cell’s genome.
It turns out that this process is regulated by post-transcriptional control elements, which are specific sequences within the virus that regulate RNA splicing, export, stability, and packaging into progeny virions. These regulating factors have important roles in virions’ ability to replicate and grow, and they also help the virions evade cellular defense mechanisms.
These regulating factors also help the viral genome integrate into host chromosomal DNA and create a fusion protein, which is called the v-Fps/Fes form. This fusion protein, which has lost its N-terminal sequence of Fps, is still capable of producing the viral genes that make up the virions.